توضیحات
Psoas hitch
Introduction
In the middle of the last century, Dolff [1], Paquin [2]
and Zimmermann et al. [3] developed principles for
ureteroneocystostomy after gynaecological ureter injuries.
Turner-Warwick andWorth [4] adopted these techniques,
named it the ‘Psoas Bladder-Hitch Procedure’ and applied
this technique of ureteroneocystostomy for the treatment
of distal ureteric obstruction, ureteric fistulas and ‘distended
duplication’ of the upper urinary tract.
This technique includes three major advantages for a
complex ureteroneocystostomy: i) Mobilisation of the
bladder with fixation above the iliac vessels to guarantee a
tension-free ureteric anastomosis; ii) Formation of an
adequate submucosal tunnel to prevent VUR; iii)
Implantation of the ureter into an immobilised part of the
bladder to prevent kinking during filling and emptying of
the bladder [5, 6].
In contrast to intravesical techniques for ureteric
reimplantation, the psoas hitch procedure is also well
suited for children with megaureters, as it can be
combined with mobilisation of the ureter up to the kidney,
so that secondary kinking of the ureter can be resolved.
Tapering of a megaureter is rarely required, given that the
diameters of the middle and proximal thirds of the ureter
are usually smaller than that of the distal part, permitting
creation of a submucosal tunnel for anti-refluxing ureteric
implantation.
The psoas (bladder) hitch technique is an almost universal
approach for ureteric reimplantation whatever the problem
of the distal ureter. If this technique is not possible, an
additional Boari flap may be useful
At the end of the nineteenth century, Boari described a
bladder flap substitution of the distal ureter [7]. The
surgical technique was developed to bridge lesions of the
distal ureter arising from surgical interventions (mainly
gynaecological complications) or tuberculosis [8–11]. A
modification by Übelhör is a deviation from the formal flap
technique.
Planning and Preparation
Indications
High-grade reflux with dilated ureter not suitable for an
extravesical reimplantation.
• Obstructive and/or refluxive megaureter.
• Double system not suitable for extravesical
reimplantation.
• Distal ureteric defects up to 5–8 cm above the ureteric
orifice (for higher defects an additional Boari-flap may be
used).
• Ureteric trauma, ureteric fistula, obstruction of the distal
ureter or distal(solitary, low grade) urothelial cancer of
the ureter.
Specific Instruments and Materials
Optical loupes (2.5–3.5, 50-cm focal length).
• Small Langenbeck retractors.
• 6/0 or 7/0 glyconate monofilament absorbable sutures for
ureteric reimplantation (Monosyn® or Monocryl®).
• 4/0 and 5/0 poly-p-dioxanone monofilament absorbable
sutures (e.g.Monoplus® or PDS®) for bladder closure.
4/0 or 5/0 glyconate or polyglytone monofilament rapidly
absorbable sutures for fixation of stents, cystostomy (e.g.
Monosyn Quick® or Caprosyn®).
• 3/0 poly-p-dioxanone monofilament absorbable sutures
(e.g.Monoplus® or PDS®) for bladder fixation at the
psoas muscle.
• 4, 6 or 8 F polyurethane/polypropylene ureteric stents.
• 10 F pigtail cystostomy catheter.
Patient Preparation
Confirmation of adequate bladder capacity should be
obtained preoperatively to allow a tension-free
anastomosis.
In patients with severe ureteric pathology, which might
extend towards the middle or upper third of the ureter,
bowel preparation is advisable in the event of intestinal
ureter substitution becoming necessary.
Acute UTI must be treated preoperatively.
Patient Positioning
The patient is placed supine on the table with ª15 °
overextension. A Foley transurethral catheter is inserted,
which must provide intraoperative access for filling the
bladder during the operation
Figure 1
A supra-inguinal ‘hockey stick’ incision is made
where the length of the cranial extension
(hockey stick handle) depends on the patient's
size and the expected length of the ureteric
defect. In cases with an unexpected length of
pathology, a primary smaller incision may be
extended cranially as needed.
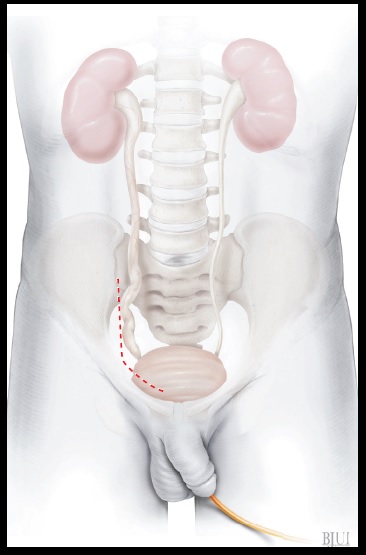
Figure 2
The ureter is exposed through an extraperitoneal
approach. After division of the inferior epigastric
vessels and, in female patients, division of the
round ligament of the uterus (in males
mobilisation the spermatic cord and the
spermatic vessels), the medial umbilical
ligament (umbilical artery) is identified. If there is
severe scarring after previous surgery or
radiotherapy, the ureter is most readily identified
behind the branching of the umbilical artery
from the hypogastric artery (internal iliac artery)
or alternatively at its crossing with the common
iliac artery. The ureter is lifted up by a vessel loop
to ease further preparation. Care must be taken
to preserve the periureteric adventitial tissue with
its inherent blood supply of the ureter.
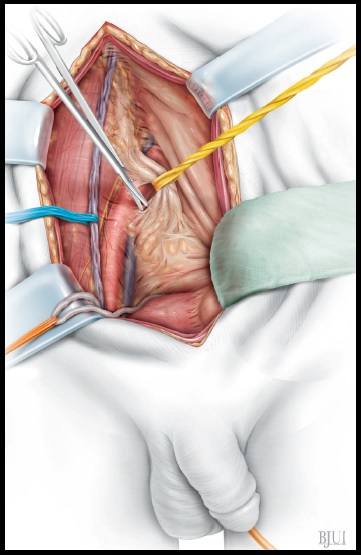
Figure 3
The ureter is mobilised towards to the bladder as
far as possible, transected and its distal stump
ligated. In cases with a ureteric fistula or an
iatrogenic obstruction, the ureter is transected
above that level. A stay suture is placed into the
proximal ureteric stump at the 6 o'clock position.
The ureter is carefully mobilised cranially to avoid
any injury to the longitudinal ureteric vessels. In
patients (mostly children) with an obstructive
megaureter, the middle and/or proximal third of
the ureter are usually smaller in diameter than
the distal third and can be re-implanted without
tailoring in most cases.
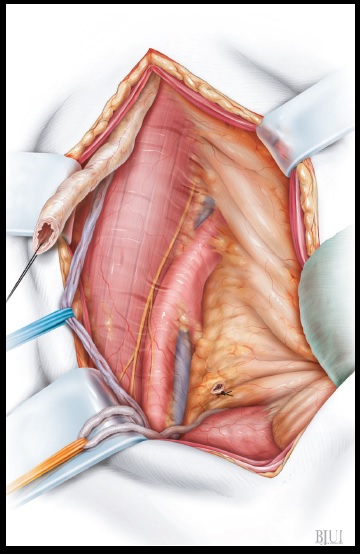
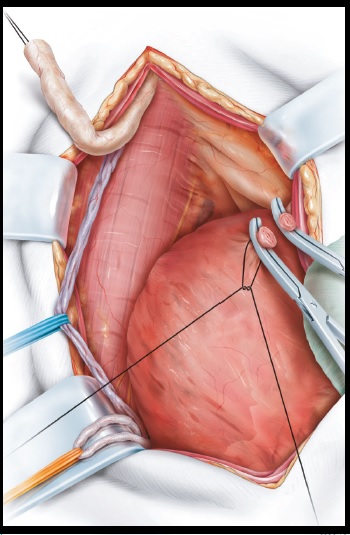
Figure 4
Before commencing its mobilisation, the bladder
is filled with 50 mL (infants) to 200–300 mL
(adults) of saline through the Foley catheter to
ease dissection. The peritoneum is dissected
from the surface of the bladder. In patients with
a long ureteric defect extending higher up,
bladder mobilisation is extended and both the
median umbilical ligament (urachus) and the
ipsilateral medial umbilical ligaments (and
occasionally also the contralateral medial
umbilical ligament) have to be divided. The aim
is to allow a tension-free fixation of the bladder
at the psoas muscle at least 2–3 cm above the
common iliac vessel.
Psoas hitch and Boari flap
ureteroneocystostomy
Raimund Stein, Peter Rubenwolf, Christopher Ziesel, Mohamed M. Kamal* and
Joachim W. Thüroff*
Division of Paediatric Urology and *Department of Urology, University Medical Center, Johannes Gutenberg
University, Mainz, Germany
ILLUSTRATIONS by STEPHAN SPITZER, www.spitzer-illustration.com